Content Summary
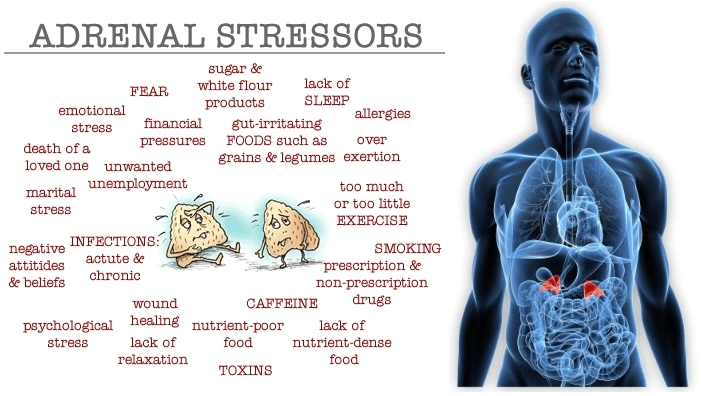
Adrenal insufficiency, a disorder characterized by underactive adrenal glands, unveils a cascade of challenges stemming from insufficient production of vital hormones, primarily cortisol and, in some cases, aldosterone.
Nestled on top of each kidney, the adrenal glands, composed of the inner medulla and outer adrenal cortex, play a pivotal role in maintaining hormonal equilibrium crucial for the body's overall well-being.
In the intricate dance of the endocrine system, the hypothalamus, pituitary glands, and adrenal glands collaborate harmoniously to orchestrate the production of hormones, orchestrating a symphony that regulates various body systems.
This delicate balance is imperative for sustaining health, and any disruption in the signaling and feedback mechanism can lead to significant disruptions and illness.
Roles of Cortisol and Aldosterone
Cortisol - The Multifaceted Regulator
Cortisol, a glucocorticoid hormone emanating from the adrenal cortex, dons many hats in the intricate ballet of bodily functions. Its roles span across the metabolism of carbohydrates, proteins, and fats.
Beyond these metabolic functions, cortisol actively participates in regulating blood glucose levels, acts as a potent anti-inflammatory agent, and steers the body's responses to stress. Its absence or insufficiency can trigger a cascade of imbalances, affecting various physiological processes.
Aldosterone - The Salt and Potassium Maestro
Aldosterone, another essential hormone produced by the adrenal cortex, assumes the role of a mineralocorticoid. Its primary responsibility lies in managing the delicate balance of salt and potassium in the blood.
This equilibrium is crucial for maintaining proper blood pressure levels and ensuring the body's effective response to stressors. In the absence of adequate aldosterone, the body grapples with weakness, dehydration, and an inability to sustain optimal blood pressure.
Prevalence and Impact
Adrenal insufficiency, while not a pervasive disorder, impacts a significant number of individuals, with an estimated prevalence of 1-4 people per 100,000. This condition does not discriminate based on age or gender, affecting patients across diverse demographics. Both males and females stand equally susceptible to the challenges posed by adrenal insufficiency.
As a disorder intricately linked to the intricate hormonal dance within the body, adrenal insufficiency requires careful management and intervention. The recognition of its symptoms and prompt diagnosis are paramount for ensuring effective treatment strategies. Individuals grappling with adrenal insufficiency often experience symptoms such as fatigue, weakness, dehydration, and difficulties in responding to stress.
Decoding Adrenal Insufficiency: A Comprehensive Exploration and Diagnostic Insights
As we delve deeper into the intricate realm of adrenal insufficiency, it becomes imperative to unravel the diagnostic tools that enable healthcare professionals to navigate this complex terrain.
Laboratory tests play a pivotal role in discerning the status of adrenal function and identifying key hormonal imbalances. Here, we shed light on the essential diagnostic tests integral to understanding and managing adrenal insufficiency.
- Cortisol Levels:
Cortisol, the cornerstone hormone produced by the adrenal cortex, undergoes scrutiny through blood tests. Given its natural peak in the early morning, consistently low cortisol levels may indicate adrenal gland dysfunction or insufficient stimulation by adrenocorticotropic hormone (ACTH). This, in conjunction with ACTH and ACTH stimulation tests, aids in the diagnosis of adrenal insufficiency. - ACTH Baseline Test:
Adrenocorticotropic hormone (ACTH), originating from the pituitary gland, signals the adrenal glands to release cortisol. A baseline ACTH test serves as an initial evaluation of pituitary function. Low ACTH levels point towards secondary adrenal insufficiency, while elevated levels may signify primary adrenal insufficiency, as seen in Addison’s disease. This test often complements the ACTH stimulation test. - ACTH Stimulation Test:
The ACTH stimulation test involves measuring cortisol levels before and after administering synthetic ACTH. A functional adrenal gland responds by increasing cortisol levels post-ACTH injection. Minimal response indicates adrenal gland damage, aiding in the diagnosis of adrenal insufficiency. - Aldosterone Levels:
Blood or urine tests measuring aldosterone levels contribute to diagnosing Addison’s disease. Low aldosterone levels suggest potential primary adrenal insufficiency, providing crucial diagnostic insights. - Electrolyte Measurement:
Electrolytes, encompassing sodium, potassium, chloride, and bicarbonate, undergo an assessment to detect and evaluate the severity of electrolyte imbalances. Addison’s disease often manifests with low sodium, chloride, and bicarbonate levels, coupled with elevated potassium levels. - Urea and Creatinine:
Monitoring kidney function is integral in adrenal insufficiency management. Urea and creatinine tests serve as valuable indicators, ensuring the kidneys function optimally during the diagnostic and treatment phases. - Glucose Levels:
During an Addisonian crisis, glucose levels may plummet. Monitoring glucose levels is crucial for crisis management, offering insights into the patient's overall condition during critical episodes.
Understanding the intricacies of adrenal insufficiency requires a comprehensive diagnostic approach. These laboratory tests serve as indispensable tools, guiding healthcare professionals in deciphering hormonal imbalances, identifying adrenal dysfunction, and formulating tailored treatment strategies.
As technology and medical knowledge advance, these diagnostic measures continue to play a pivotal role in enhancing our understanding and management of adrenal insufficiency.

Deciphering the Enigma: Signs and Symptoms of Adrenal Insufficiency
Adrenal insufficiency, a complex disorder marked by underactive adrenal glands, manifests through a spectrum of symptoms that may initially be subtle and non-specific.
The progression of these symptoms often unfolds gradually, gaining momentum during periods of heightened stress and intensifying over months. Here, we unravel the diverse signs and symptoms associated with adrenal insufficiency.
- Fatigue and Weakness:
Overwhelming fatigue and weakness are hallmark indicators, permeating through daily life and compromising overall vitality. - Abdominal Pain:
Vague abdominal discomfort may surface, contributing to the overall discomfort experienced by individuals with adrenal insufficiency. - Dehydration (Addison’s Disease):
Addison’s disease, a specific form of adrenal insufficiency, may present with dehydration as a distinctive symptom. - Gastrointestinal Distress:
Symptoms such as diarrhea or constipation may emerge, impacting the digestive equilibrium and adding to the multifaceted nature of adrenal insufficiency. - Dizziness and Fainting:
Individuals may experience episodes of dizziness and fainting, underscoring the systemic impact of adrenal dysfunction. - Hyperpigmentation (Addison’s Disease):
Unique to Addison’s disease, hyperpigmentation manifests as dark patches, often concentrated in skin folds. Black freckles on the forehead and face, along with discoloration around areas like the nipples, lips, and rectum, may also be observed. - Joint and Muscle Aches:
Aches in joints and muscles contribute to the overall physical discomfort associated with adrenal insufficiency. - Low Blood Pressure:
Hypotension, or low blood pressure, is a common symptom, reflecting the regulatory role of adrenal hormones in blood pressure maintenance. - Hypoglycemia:
Fluctuations in blood sugar levels may lead to hypoglycemia, contributing to symptoms such as shakiness, irritability, and confusion. - Salt Craving (Addison’s Disease):
Addison’s disease may evoke an unusual craving for salt, reflecting imbalances in mineralocorticoid hormones. - Vomiting:
Episodes of vomiting may occur, adding to the gastrointestinal challenges experienced by individuals with adrenal insufficiency. - Weight Loss:
Unexplained weight loss may be noted, underscoring the metabolic impact of adrenal dysfunction. - Decreased Body Hair:
Changes in body hair may occur, reflecting the broader influence of adrenal hormones on skin and hair health.
Adrenal Crisis (Addisonian Crisis):
In some cases, adrenal insufficiency may progress to an acute crisis, constituting a medical emergency. Key symptoms during an adrenal crisis may include:
- Low Blood Pressure:
A precipitous drop in blood pressure is a critical feature of an adrenal crisis. - Severe Pain:
Intense pain in the lower back, abdomen, or legs may manifest, indicating the severity of the crisis. - Vomiting and Diarrhea:
Severe gastrointestinal symptoms, including persistent vomiting and diarrhea, can lead to dehydration and exacerbate the crisis. - Shock:
The body may enter a state of shock, with a cascade of physiological responses impacting multiple organ systems. - Kidney Failure:
Acute adrenal failure may lead to kidney dysfunction, further escalating the crisis. - Loss of Consciousness:
In advanced stages, individuals may experience loss of consciousness, necessitating immediate medical intervention to avert potential fatality.
Understanding these nuanced signs and symptoms is pivotal in the timely identification and management of adrenal insufficiency, ensuring optimal care for affected individuals.
Conclusion
In conclusion, adrenal insufficiency underscores the profound impact of hormonal balance on overall health. The collaboration of the hypothalamus, pituitary glands, and adrenal glands serves as a testament to the intricate nature of the body's regulatory systems.
Understanding and addressing adrenal insufficiency not only offers insights into the complexities of the endocrine system but also paves the way for tailored interventions to restore hormonal equilibrium and foster well-being.
Regulate Your Cortisol Levels with Laminine from Lifepharm
How does Laminine lowers cortisol in your body:
Get your Laminine today and enjoy a healthy mind and body!

Relevant Reads>>>